Everyone has nights when sleep won't come. You toss and turn, watch the clock, and wonder why your brain won't shut off. But when does a bad night become something more serious?
Insomnia isn't just poor sleep. It's a medical condition with specific symptoms that affect your entire day, not just your nights. If you're feeling broken by exhaustion, you might be looking for answers about what's happening to your body.
What Makes Insomnia Different from a Bad Night?
Clinical insomnia follows what doctors call the "3-and-3 Rule." You have difficulty sleeping at least 3 nights per week for 3 months or longer. According to research published by the National Library of Medicine, this pattern affects 6-10% of adults who meet strict diagnostic criteria, while 30-36% report at least one insomnia symptom.
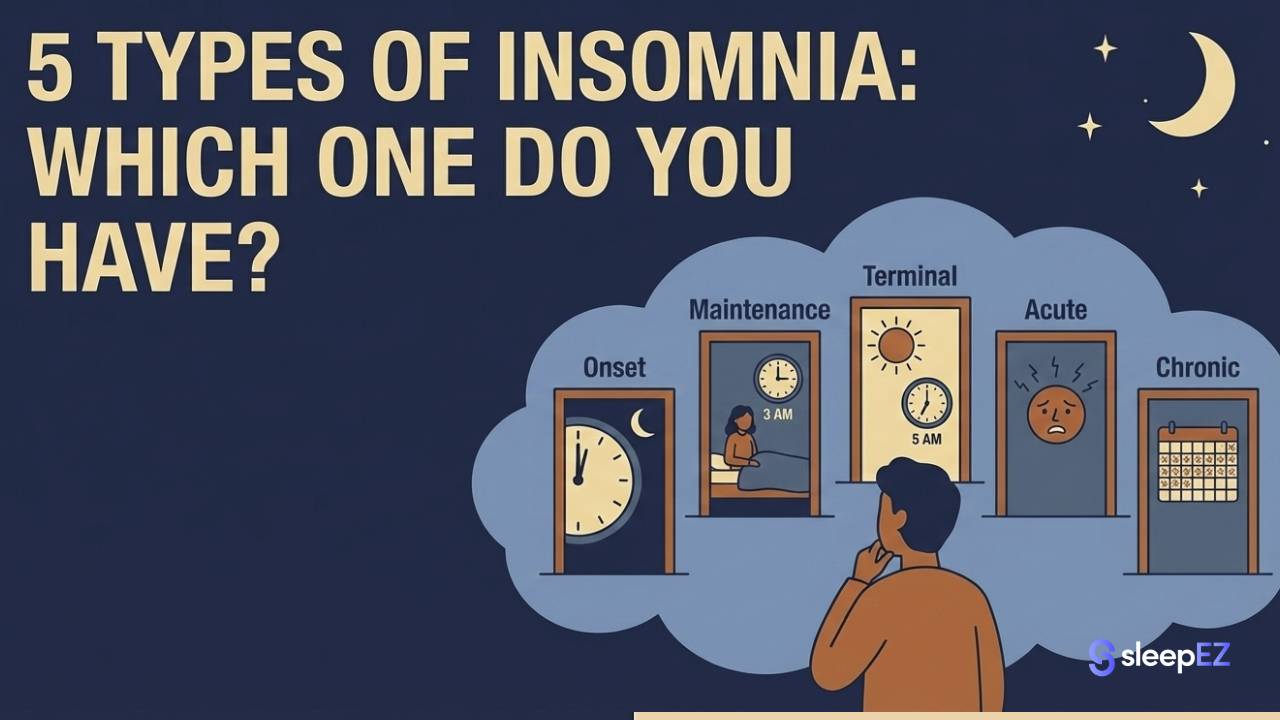
There are two main types:
Acute insomnia lasts less than 3 months. It's usually triggered by stress, travel, or a major life event. Your sleep patterns return to normal once the trigger passes.
Chronic insomnia persists for 3 months or more. Your body has learned poor sleep patterns that continue even when the original stress is gone. This type requires treatment to break the cycle.
The Nighttime Symptoms: The "Can't Sleep" Phase
1. You Take Forever to Fall Asleep
If you regularly take more than 30 minutes to fall asleep, that's a red flag. Sleep doctors call this "sleep onset latency." You lie in bed feeling tired, but your mind stays active and your body won't relax.
2. You Wake Up Multiple Times
This is called "sleep maintenance insomnia." You might fall asleep fine, but then you wake at 2 a.m., 4 a.m., and 5 a.m. Each time, you struggle to drift back off. Your sleep feels broken into pieces instead of one solid block.
3. You Feel "Tired but Wired"
This is hyperarousal, one of the hallmark symptoms of insomnia. Studies from the National Institutes of Health show that hyperarousal may be a causal factor in chronic insomnia. Your body is exhausted but your nervous system stays in high alert mode.
Your eyes stay wide open. Your heart might race. Small sounds become impossible to ignore. A distant car alarm or a partner's breathing suddenly feels unbearably loud.
Insomnia often makes you hypersensitive to your environment. A streetlight or distant noise that wouldn't bother a normal sleeper becomes unbearable. Using blackout sleep masks and noise-reducing earplugs helps dampen this sensory overload, signaling to your brain that it is safe to power down.
The Daytime Symptoms: The "Zombie" Phase
Here's what many people don't realize: insomnia is a 24-hour disorder. The symptoms don't stop when the sun comes up. Your daytime struggles are just as important for diagnosis as your nighttime problems.
4. You Experience Heavy Fatigue (Not Just Sleepiness)
There's a difference between fatigue and sleepiness. Sleepiness means you're fighting to keep your eyes open. Fatigue means your whole body feels heavy and drained, but you still can't sleep even if you try to nap.
People with insomnia often feel fatigue without sleepiness. You're exhausted but not drowsy. This confusing state leaves you feeling stuck between being tired and being unable to rest.
5. Your Brain Feels Foggy
Cognitive problems are a major symptom of insomnia. You might:
- Forget common words mid-sentence
- Struggle to focus on simple tasks
- Take much longer to make basic decisions
- Read the same paragraph three times without absorbing it
This mental fog affects your work, your relationships, and your confidence. You know you're capable of more, but your brain won't cooperate.
6. Your Body Starts to Hurt
Sleep loss creates physical symptoms that surprise many people. Common problems include:
- Tension headaches that won't go away
- Tight, sore muscles in your neck and shoulders
- Stomach problems like nausea or digestive issues
- A general sense of physical discomfort
The anxiety of insomnia often bleeds into the day. If you experience racing thoughts or trouble focusing in silence, this is a symptom of an overactive nervous system. Using a white noise sound machine during work or relaxation time can help mask distractions and lower your baseline anxiety levels.
Is It Insomnia or Sleep Apnea? The Critical Check
Many people confuse insomnia with sleep apnea, but they're different conditions that need different treatments. Sleep apnea is a breathing disorder where your airway closes during sleep. Insomnia is a problem with your brain's ability to initiate and maintain sleep.
Research shows that 39-58% of sleep apnea patients also report insomnia symptoms, while 29-67% of insomnia patients show signs of sleep apnea. The conditions often overlap, which is why proper diagnosis matters.
Here's how to tell them apart:
| Symptom | Insomnia | Sleep Apnea |
|---|---|---|
| Main complaint | Can't fall asleep or stay asleep | Always tired despite "sleeping" |
| Snoring | Rare | Very common and loud |
| Gasping for air | No | Yes, especially at night |
| Morning headaches | Sometimes | Very common |
| Dry mouth on waking | No | Yes, very dry throat |
| Energy after caffeine | Some improvement | Little to no improvement |
| Feeling sleepy | Not usually | Constant drowsiness |
Pay attention to your mouth when you wake up. Do you have a dry, scratchy throat? This is a symptom of open-mouth breathing or snoring. While mouth tape can encourage nasal breathing and reduce dry mouth, you must report this specific symptom to your doctor to rule out Obstructive Sleep Apnea (OSA).
If you snore loudly, gasp for air, or feel drowsy all day despite spending 8 hours in bed, you likely have sleep apnea, not insomnia. Both conditions are serious, but apnea can be life-threatening if left untreated.
Do Symptoms Differ by Gender?
Women Experience Insomnia Differently
Women report insomnia at rates 40% higher than men. According to peer-reviewed research in the National Library of Medicine, women are 41% more likely to experience insomnia symptoms. This gap appears at puberty, when young women face almost three times the risk compared to adolescent boys.
Why the difference? Hormones play a major role:
- During menstruation: Progesterone drops right before your period, which can disrupt sleep. Many women report worse sleep in the days leading up to menstruation.
- During pregnancy: Hormonal shifts, physical discomfort, and anxiety about the baby all contribute to sleep problems. Sleep maintenance insomnia is especially common.
- During perimenopause and menopause: Hot flashes, night sweats, and hormonal changes make falling asleep and staying asleep much harder. Studies show that female hormonal transitions including the luteal phase, pregnancy, and menopause correspond with increased risk for sleep disorders.
Women with insomnia often wake up feeling hot, anxious, or both. This is "sleep maintenance insomnia," where falling asleep isn't the problem but staying asleep is.
Men can get insomnia too, but they're more likely to have sleep apnea as the underlying cause of their sleep problems.
When to See a Doctor
Don't wait months or years to get help. See a doctor if:
- Your symptoms last more than 3 months (chronic insomnia)
- You feel drowsy while driving or operating machinery
- You gasp for air or stop breathing during sleep (possible apnea)
- Your sleep problems are affecting your work, relationships, or safety
- You've tried improving your sleep habits but nothing helps
Insomnia is treatable. Cognitive behavioral therapy for insomnia (CBT-I) works better than sleeping pills for long-term relief. Other treatments include medication, light therapy, and addressing underlying health conditions.
Listen to Your Body's Signals
Insomnia shows up in both your nights and your days. If you have trouble falling asleep, wake up frequently, and feel foggy and exhausted during the day, those are symptoms of a medical condition, not a personal failure.
The "3-and-3 Rule" is your guide: 3 nights per week for 3 months means it's time to take action. Pay attention to whether you're just tired or if you're also snoring and gasping, which points to sleep apnea instead.
Don't guess about what's happening to your body. Start tracking your symptoms both day and night. Note when you go to bed, how long it takes to fall asleep, how many times you wake up, and how you feel the next day. This information will help your doctor make an accurate diagnosis.
Your sleep problems are real, they're measurable, and they're fixable. The first step is recognizing that what you're experiencing has a name and a treatment plan. You don't have to live like this.
This article is for information only. It doesn't replace medical advice. Always talk to a doctor about sleep problems before starting treatment.


Leave a comment
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.